Description
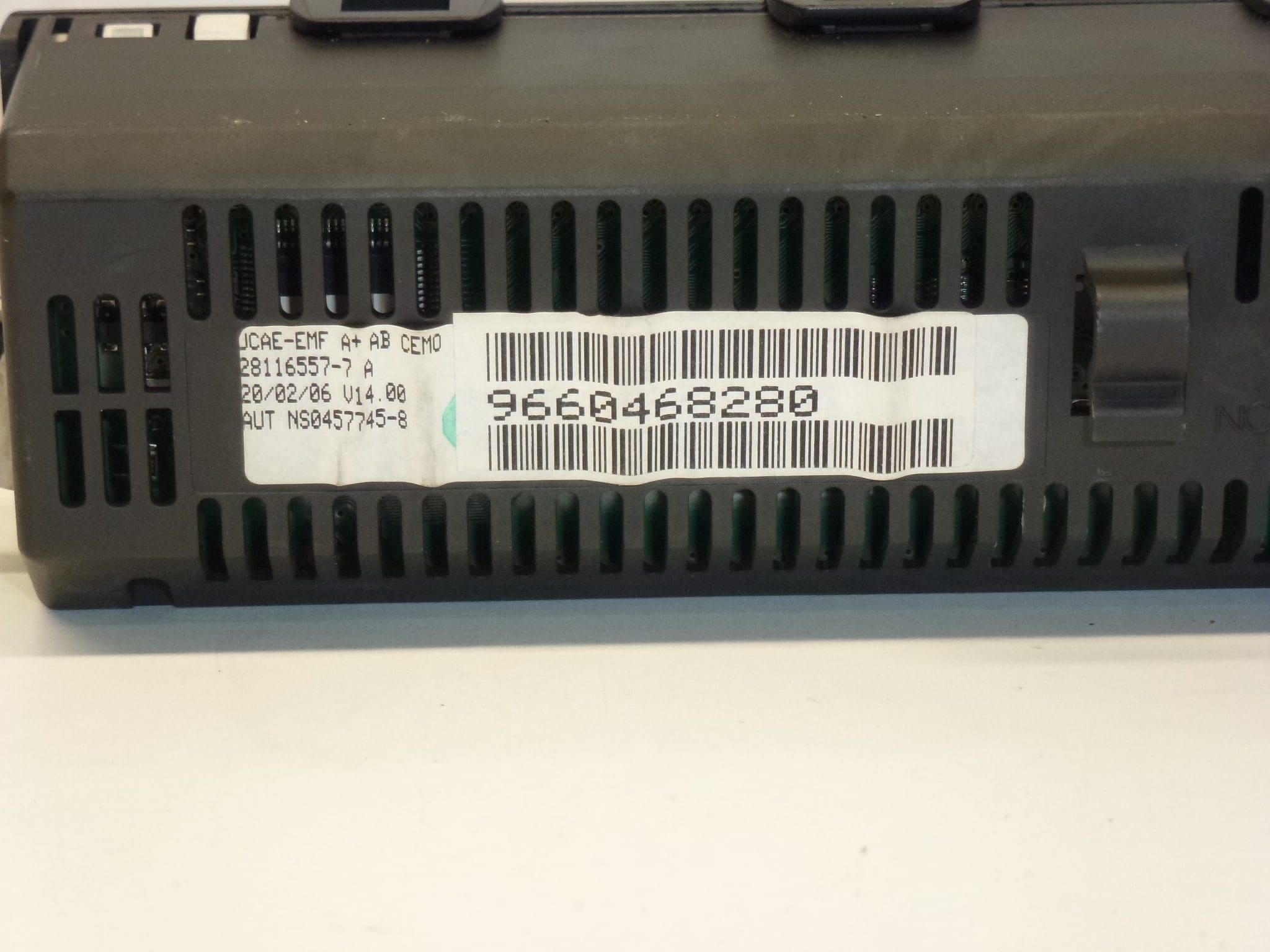
Affichage de la radio, de l’ordinateur de bord et de la climatisation monozone Citroën C5 première génération facelift Il peut être nécessaire de configurer avec votre voiture, je recommande de suivre la référence 9660468280 Citroën C5 est une voiture de milieu de gamme qui est produite depuis 2001 à nos jours La production des voitures Citroën C5 de la première génération a eu lieu en 2001 – 2003, le lifting a été produit de 2003 à 2008. La production des voitures de la deuxième génération a eu lieu dans les années 2008-2010, le lifting de la la deuxième série a été produite de 2010 à 2017. 2021 et toujours produite aujourd’hui Lors de la commande, vous avez la possibilité d’entrer le numéro VIN et nous vérifierons la compatibilité de la pièce avec votre voiture.
Comment remplacer l’écran ?
L’écran est fixé à la carte avec deux vis THORX 20
Fabriquant de pièces: JOHNSON CONTROLS
Johnson Controls est un leader technologique et industriel mondialement diversifié au service de clients dans plus de 150 pays. Nos 150 000 collaborateurs créent des produits, services et solutions de qualité pour optimiser l’efficacité énergétique et opérationnelle des bâtiments ; Batteries automobiles au plomb et batteries avancées pour véhicules hybrides et électriques ; et systèmes intérieurs pour automobiles. autres codes 9660468280 6155FV